Blood Sugar Fluctuations: Should You Worry About Them?
|
|
8 min
|
|
8 min
Many people with diabetes get blood sugar fluctuations. It could be right after eating, exercising, or throughout the day.
These fluctuations are usually not dangerous. However, abnormal blood sugar swings can cause some unexpected complications. This guide will provide a more in-depth look at this.
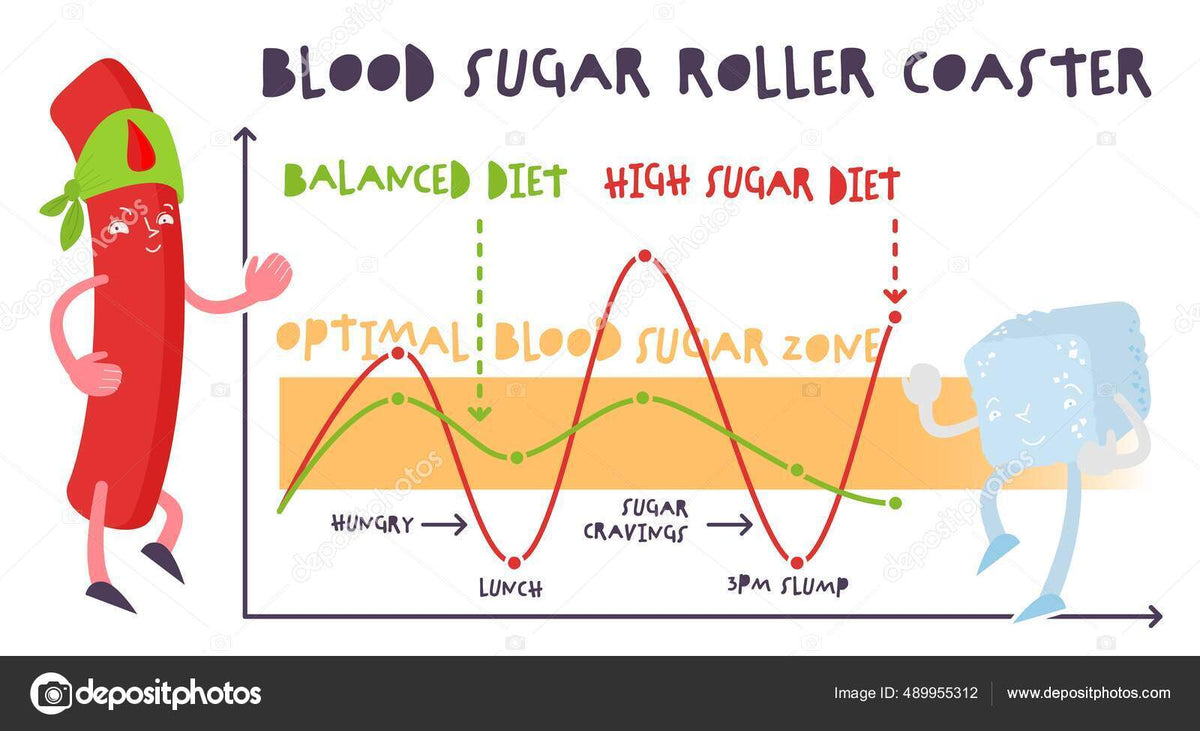
Blood sugar fluctuations are rapid changes in the blood glucose levels throughout the day.
Usually, your blood sugar levels rise after a meal and gradually decrease until your next meal. This is a normal, healthy change of blood sugar levels.
In abnormal cases, the fluctuations become more prominent, leading to excessive highs and lows that negatively affect your health.
Blood glucose fluctuations can be dangerous due to large spikes in short intervals.
This is harmful for people with diabetes since they’re more vulnerable to these blood sugar swings.
Constant fluctuations result in a condition known as brittle diabetes, where the person’s blood sugar level alternates between hyperglycemia (too high) and hypoglycemia (too low).
The primary reason for blood sugar fluctuations is diabetes (both type 1 and type 2). Other reasons for blood sugar fluctuations include dehydration, extreme weather, eating too much sugar at one go, or vigorous exercise.
We can divide the fluctuations into three categories:
Processed foods, high-carbohydrate, sports drinks, sodas, and sugary foods can increase blood sugar.
Blood glucose usually increases after a meal, but these sugar-rich foods will increase blood sugar levels even more.
When your body is fighting off an infection, it’ll raise the blood sugar levels to help your cells fight it.
The release of stress hormones, like cortisol, and inflammatory molecules (prostaglandins) mediates this process.
Strenuous exercise, getting lost, or stressing over any stimulant causes the release of stress hormones in the body. Cortisol and adrenaline are among the stress hormones released to boost your energy when excessive stress triggers your fight or flight response.
However, these hormones also make it harder for insulin to allow cells to utilize the sugar in the bloodstream, leading to hyperglycemia.
Some medications, like dexamethasone, can increase blood sugar levels by interfering with the insulin’s ability to move sugar from your bloodstream into the cells.
Corticosteroids, like prednisone, are known to increase blood sugar levels to a higher limit compared to other medications. In some cases, these steroids contribute to developing diabetes in people who didn’t have it before.
When a person with no preexisting conditions stops drinking water (or any fluids) for a prolonged period, the amount of fluid in their plasma decreases while the amount of sugar remains the same. This causes a relative spike in their blood glucose levels.
Longer periods without eating will hinder your body’s ability to maintain stable blood glucose. Making a habit of skipping meals can induce a hypoglycemic episode, even if you’re not on insulin or antidiabetic medication.
Excessive exercise, especially if not accompanied by sufficient hydration and food intake, can deplete your body’s stored sugar faster. Some people mix vigorous workouts with prolonged fasting or crash dieting in hopes of rapidly losing weight.
While these people do end up losing some weight, a large amount of lost weight is often from their muscle mass. When the liver’s glucose storage is depleted, it breaks down the muscles to produce energy, a process known as muscle catabolism.
Among the most common diseases that cause blood glucose level reduction are hypothyroidism and Addison’s disease.
Hypothyroidism affects the thyroid gland, preventing it from secreting enough thyroid hormone. The lack of this hormone can slow down the metabolism and affect blood sugar regulation, causing chronic hypoglycemia.
On the other hand, Addison’s disease affects the adrenal glands and prevents them from secreting enough cortisol, which is another hormone that plays a role in blood sugar regulation.
The liver acts as a carbohydrate storage organ for the body. A healthy liver stores extra sugar after meals, in the form of glycogen, and releases it between meals. It can even, to some extent, synthesize new sugar when needed.
This regulatory mechanism is disrupted when the liver isn’t healthy. Liver diseases, like hepatitis, fatty liver disease, and cirrhosis, can cause unpredictable fluctuations between low and high blood sugar levels, leading to various complications.
Extreme cold or hot temperatures can fluctuate your blood glucose levels. Excessive heat can put our bodies under stress, releasing stress hormones that reduce the effect of insulin and increase blood sugar levels. This effect is further accentuated by dehydration.
Yet, the same hot weather can cause a decrease in blood sugar levels if the person takes insulin.
Similarly, the body can release stress hormones when it’s too cold. Yet, if the person is skipping meals or is low on blood sugar, the cold can mask the effects of hypoglycemia.
This high unpredictability makes it highly recommended to avoid weather extremes, especially for people with diabetes.
Alcohol can induce a roller coaster of blood glucose levels because of the variation of how different individuals can process it. Alcoholic drinks typically contain a lot of carbs, which causes a spike in blood glucose after ingestion.
Yet, hours later, the level may drop suddenly because the liver prioritizes alcohol breakdown over other tasks. This effect differs from person to person based on age, condition of the liver, and the amount of alcohol ingested.
It’s challenging to predict blood sugar levels after drinking alcohol. As such, it’s best to minimize drinking. If you do drink, it’s best to do so with food, keep the amount you drink down to 14 units of alcohol per week spread over 3 or 4 days, and avoid binge drinking.
Hormone regulation gets severely disrupted during menstruation and pregnancy, leading to various physical symptoms.
Since blood glucose levels are heavily influenced by hormonal release, this disruption can also cause them to either get too high or too low without a predictable pattern.
It’s strongly recommended for pregnant and menstruating women to check their blood sugar daily, especially if they’re at risk of developing diabetes.
The symptoms of low blood sugar include, but are not limited to:
Meanwhile, the symptoms of high blood sugar include:
The constant switch between high and low blood sugar levels yields a mixture of these symptoms.
By familiarizing yourself with the reasons for fluctuations and the symptoms to look for, you can quickly notice when your blood sugar levels are out of the norm.
Pair that with a visit to your doctor, and you can isolate the reason(s) for these fluctuations.
The doctor will take a detailed medical history from you. Make sure to be honest about your eating and drinking habits, as well as your lifestyle, amount of physical exercise, medications you take, and the amount of stress present in your life.
If you have a habit of consuming sweets and sugary beverages, you should try a lower-carb diet under the supervision of your doctor.
As for prediabetic or currently diagnosed, an insulin resistance diet can be an excellent way to keep blood glucose levels stable.
Physical exercise improves your insulin resistance, balances your cholesterol levels, improves your muscle mass, and helps you lose weight.
Stress is responsible for various medical problems. As such, doing your best to eliminate it can help you restore your hormonal balance and normal body functions.
The treatment of any physical condition requires careful monitoring to evaluate the results. This is especially important in case of blood sugar fluctuations, as you may need to check them several times a day.
You can do so by using glucometers, which accurately measure your blood sugar levels. However, they may not be the best solution for those who fear needles, especially because they need to be used at least once a day.
A good alternative solution is utilizing continuous glucose monitors or CGMs, which utilize implanted sensors under the skin that are connected to an external display device.
They provide updates on the blood sugar levels at fixed intervals, usually every half a minute or every few minutes.
Sometimes, the doctor may give you some pointers on how to put your life back on track. This includes therapy to reduce stress, dietary tips, and an insulin resistance diet (if the problem is caused by type 2 diabetes).
Depending on your history and diagnosis, your doctor may also prescribe some medications and/or insulin therapy to mitigate your symptoms.
People with type 1 diabetes and other insulin-dependent diabetes usually suffer from low or interrupted insulin secretion. They rely on exogenous insulin before each meal to prevent the blood sugar levels from rising too much.
On the other hand, if they take insulin and skip a meal, their blood sugar will drop, sometimes to dangerously low levels.
As such, optimum insulin regulation is paramount to prevent blood sugar levels from fluctuating.
One of the best tools to help you safely and quickly inject insulin when you need to is the InsuJet injector.
InsuJet injectors don’t have a needle unlike traditional needles and insulin pens. Besides making the process much easier for people who fear needles.
It’s compatible with all U-100 insulins, draws doses accurately, and minimizes environmental impact by eliminating the need for needles. You can use the same injector up to 5,000 times.
Blood sugar fluctuations can lead to unpredictable side effects, some of which could be dangerous. It’s important to identify the cause(s) behind these fluctuations with the help of a doctor so you can maintain adequate blood sugar control.
Follow your doctor’s advice, stay active, and avoid harmful foods that can spike your blood sugar levels. As for people with insulin-dependent diabetes, safely administering daily insulin using a needle-free InsuJet is a good approach to maintain adherence to your insulin therapy.






 InsuJet injector into midsection" data-srcset="https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_1800x.png?v=1704935718 1800w, https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_1600x.png?v=1704935718 1600w, https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_1400x.png?v=1704935718 1400w, https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_1200x.png?v=1704935718 1200w, https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_1000x.png?v=1704935718 1000w, https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_800x.png?v=1704935718 800w, https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_600x.png?v=1704935718 600w, https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_400x.png?v=1704935718 400w">
InsuJet injector into midsection" data-srcset="https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_1800x.png?v=1704935718 1800w, https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_1600x.png?v=1704935718 1600w, https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_1400x.png?v=1704935718 1400w, https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_1200x.png?v=1704935718 1200w, https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_1000x.png?v=1704935718 1000w, https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_800x.png?v=1704935718 800w, https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_600x.png?v=1704935718 600w, https://cdn.shopify.com/s/files/1/1596/5421/files/blog-image-1704935713389_png_400x.png?v=1704935718 400w">